Imagine you are a 1st-year emergency medicine resident. Your attending is on call for the night shift you are working, and you are about to see your very first patient on your own. Before entering the room you read in the chart: 65 y/o cis-gendered woman presents with chief concern of chest pain that has been constant for 3 days.
You ask yourself, what could be going on? What should I prepare for before I see the patient? You quickly start to formulate your differential diagnosis, a list of possible diagnoses that could explain the patient’s chief concern and story.
 An intimidating part of being a new medical student is figuring out how to come up with a differential diagnosis for the patient sitting in front of you. There are so many questions running through our minds as we learn more clinical skills and knowledge that it can be overwhelming to know where to begin with a patient presenting with shortness of breath, stomach pain, or chest pain. That is where the Chief Concern Course comes in!
An intimidating part of being a new medical student is figuring out how to come up with a differential diagnosis for the patient sitting in front of you. There are so many questions running through our minds as we learn more clinical skills and knowledge that it can be overwhelming to know where to begin with a patient presenting with shortness of breath, stomach pain, or chest pain. That is where the Chief Concern Course comes in!
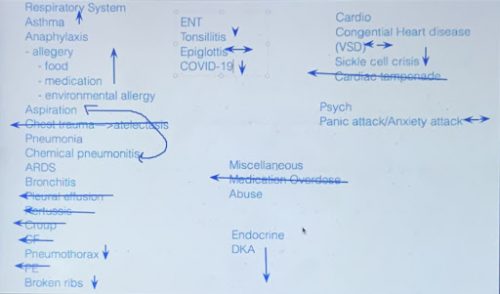
We are put in small groups of about 20 students and one faculty member physician and are provided a brief blurb about a patient. Before class, we are asked to come up with about 5 diagnoses, just like a doctor does before they see the patient. At the beginning of our virtual session, we all throw out any diagnoses we have based on the minimal information we were given in our prompt. This list is usually huge! We learned pretty quickly that some common presenting symptoms, like chest or abdominal pain, can be due to a variety of different systems — cardiovascular, pulmonary, musculoskeletal, gastrointestinal, or neurological to name a few! So without a lot of information, we have to start with a wide list. As we learn more about the patient and continue through the encounter, this list narrows. We start with asking questions and taking a patient medical history, performing a physical exam, and finally requesting labs and imaging. At the end of each session, with our monster list of diagnoses in hand, we are put into breakout rooms of smaller groups of 3-4 students to work on our next steps.
Back in the emergency department, you have developed your initial differential diagnosis, including gastrointestinal causes like cholecystitis or gastroesophageal reflux, cardiac causes like myocardial infarction or pulmonary embolism, pulmonary causes like pneumothorax, and musculoskeletal concerns like costochondritis. Now you are ready to enter the room to see the patient. What questions will you ask? What do you want to know more about? What will help you narrow down your list of diagnoses?
What additional information should we gather from the patient’s history?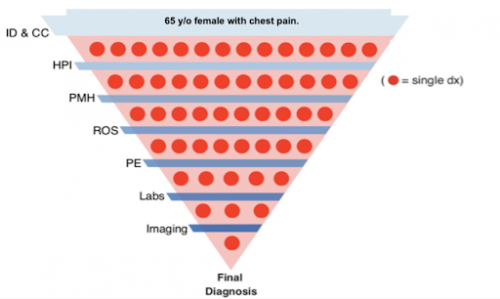
In class, imagining we are about to interview the patient, we are placed into our smaller breakout rooms for our first objective: develop a list of questions to further gather information about the patient. A critical part about being a first-year medical student is learning how to take a thorough patient history. Thankfully, throughout our Doctoring sessions (Learn more about our Doctoring course here), we have learned how to inquire about the basic patient history, which includes information about their present illness, past medical, surgical, family and social history, medications, allergies, and a detailed review of systems. While this seems like a lot at first, surprisingly the more you practice the more it becomes second nature! What Chief Concern allows us to discuss, as a group, some of the key questions we’d like to ask the patient first. Because our medical knowledge is limited, this can be really tricky to narrow down relevant questions! We have really enjoyed working together with our classmates to come up with our plan for asking the patient’s history, especially because everyone remembers different key points from lectures and has different prior experiences and knowledge they bring to the group. This makes for great discussions and always serves as a great reminder that while we may think we know the exact questions that are relevant, often there are questions that would investigate diagnoses we hadn’t even considered.
After our first small breakout groups, we come back together to now ask our faculty lead the history questions we just generated, and they provide us the answers as if they were the patient. This is where we really start to think critically about which of our diagnoses are moving up on our list and which ones we can move down as being less likely. Some groups do this in real time by using the virtual whiteboard to start prioritizing a list! Here is an example of the resulting prioritization from one of our collaborative sessions:
 What parts of the physical exam are we most interested in obtaining?
What parts of the physical exam are we most interested in obtaining?
Next, we get another opportunity to work with our breakout groups, but this time our goal is to discuss what we would be looking for in our physical exam of the patient. As we organize a list of what we’d prioritize in a physical, it helps to break it down into what pertinent positives and negatives we’d expect to find. For example, if we have a pneumothorax on our differential diagnosis for shortness of breath we would want to auscultate for absent breath sounds. If breath sounds are present that would be considered a pertinent negative for a pneumothorax.
When we return to the large group again, our faculty lead provides us with the full history and physical exam write-up. We now get to read through the most comprehensive information about our patient, and it is a great time to ask all our questions that we have about the presentation. Often, the patient case is not very clear cut or obvious, and there are multiple signs and symptoms that still fit with multiple diagnoses. This is where we now get to prepare our case (almost like a lawyer!) for what we think the top diagnoses are and what we plan to do about it, which is called the Assessment & Plan.
What imaging, labs, and/or interventions should we do to further diagnose or treat the patient?
In the emergency department or on an inpatient floor, as you are asking questions and gathering information, you will be mentally prioritizing the diagnoses, just as we did in class. In our experience in medical school, we are still honing our skills of balancing which diagnoses are most likely given the patient’s history with which diagnoses are life threatening and need to be managed urgently. This is where the assessment and plan comes into play!
The assessment is a list of just a few (about 3-5) diagnoses that are considered most important to focus on by the clinician, either because they are most likely or the most necessary to address. It includes a summary of the patient and important information discovered. Each of these diagnoses is listed with the factors that make them more likely and the factors that make them less likely. When we present our assessment to our attendings, they should be able to have a good idea of the patient’s story and key findings so far.
The plan is usually a bulleted list of interventions or diagnostic tools that creates a step-by-step guide for you or other providers to follow for the care of this patient. These tools are listed in order of what needs to be performed first and either grouped by specific symptom/problem or by organ system if the patient is in critical condition. These interventions could include things like IV fluids, medications, or even surgery. Diagnostic tools could be simple and quick like an EKG or complex and expensive like an MRI, depending on what is necessary.
After developing our assessment and plan, we come back to the large room and discuss our work as a group. It is a collaborative effort as we complement and critique each team’s work with input from both students and the faculty. It is a great opportunity to explore what it means to be a part of a healthcare team! After we each present, we are finally provided with the end to the clinical case. Our faculty runs through the results to any tests, labs, or imaging we ordered in our plans and unveils the final diagnosis. It is the end to a great full day of clinical reasoning, and we feel a little bit more prepared to reason through real patient stories in the coming years.
Put yourself back in the shoes of that first-year emergency medicine resident. Your history taking and physical exam has helped you discover the following:
History of Present Illness:
The patient’s chest pain is right-sided and radiates to her upper right shoulder and arm. She said it began 3 days ago after she ate a big helping of lasagna. She went to urgent care the next day and they gave her Pepcid AC, which didn’t help the pain at all. She then tried swallowing a baking soda mix, which also did not help the pain. She says it is really hard to get out of bed, because she can’t put weight on her right side. She denies any nausea, vomiting, shortness of breath, or lower leg swelling.
Past Medical History:
- Prediabetes x 4 years
- Gastroesophageal reflux disease (GERD) x 10 years (has not had issues in years)
- Eczema x 3 years
Family History:
- Father: died @ age 65 of cirrhosis d/t previous alcohol use
- Mother: died @ age 78 of Myocardial Infarction (MI, a.k.a. heart attack)
- Older brother: died @ age 53 of venous thromboembolism (VTE)
Physical Exam/Vitals:
- BP 132/82, HR 75, RR 15
- No audible heart murmurs or irregularities
- Normal lung sounds
- Right upper quadrant (RUQ) tenderness to palpation
- Physical exam otherwise unremarkable
As an early practice, take this information (clinical story, given possible diagnoses, and reasoning strategies) and think about which diagnoses you would include in your assessment and do some research to find out what your next steps might be for this patient. Try to develop your own assessment and plan! We hope to see you alongside us in medical school and in the clinic in coming years where you can refine these skills!
Don’t miss the next Dose of Reality.
Kayla is a first-year medical student at University of Michigan Medical School. She loves taking walks to explore Ann Arbor and find new places to study. She is actively involved in the Student Council, is excited to begin her involvement in the Ethics Path of Excellence, and loves meeting new people and exploring different disciplines in medicine.
Cameron is a first-year medical student at University of Michigan Medical School. When he isn’t tapping the spacebar, trying to get through another flashcard review, he is usually enjoying a board game with roommates or battling other UM students in an intramural sport. You can also find him dancing for Biorhythms, acting in the Smoker, or working on Student Council!
