by Kayla Meyer & Cameron Pawlik | Jan 19, 2023
After our first year of medical school, where our brains were buried in lectures, thinking about seeing real patients was exciting but also terrifying. We had so many questions about what it means to be a “clinical student”. What is rounding? What shoes do I wear in the OR? What is the electronic medical record and how do I use it? Am I supposed to bring lunch? Are there fridges? What do you mean we get “feedback”? What do our grades mean? Am I supposed to read about all my clinic patients beforehand?
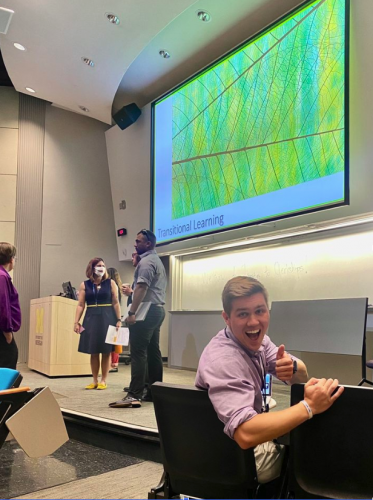
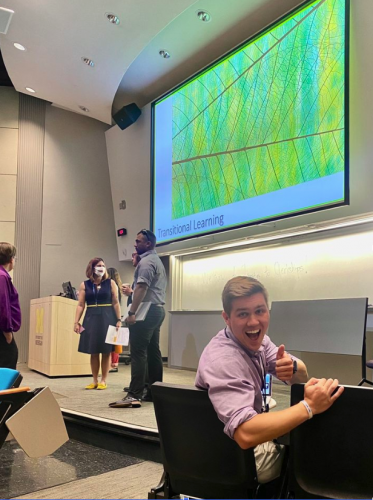
This next phase of medical school can sometimes feel like a large, looming mountain. This is why the Near Peer Program was created, to help establish mentorship early on and prepare students to feel ready to climb to the top. This program starts during Transitions to Clerkships, and continues through the academic year.
What is Transitions to Clerkships (TTC)?
 Here at the University of Michigan Medical School, our preclinical education on the basic science necessary to become a doctor is condensed into one year before we dive into the meat of medical school with the clerkship year (check out a full overview of our curriculum)!
Here at the University of Michigan Medical School, our preclinical education on the basic science necessary to become a doctor is condensed into one year before we dive into the meat of medical school with the clerkship year (check out a full overview of our curriculum)!
Before we can enter the hospital wards as effective health care team members, we need an orientation to the clinical space, and this is a month-long program called the Transitions to Clerkships (TTC). Using small group case-based discussions, clinical skills sessions and various orientation sessions, this program provides rising M2s with the experience necessary to hit the ground running in the core clerkships. These sessions range from training with the electronic health record to basic life support training. Despite this comprehensive training, the initiation to the hospital remains a difficult transition for students. Knowing this, upperclass students (M3s & M4s) started the Near Peer Program to provide the recent context of their experiences with new M2s.
What is the M-HOME Near Peer Program?
The Near Peer Program is a mentorship program linking upperclass students who have completed their clinical year with students entering their clinical year. It is under the umbrella of M-Home, which is a longitudinal learning community established to help students feel part of a “home” here at Michigan. See the blog post: Fostering Community Through my M-Home Experience.
Before the Near Peer Program ever becomes relevant and before you even start your clinical year, you are placed on a “track” via a lottery system. Your track, in the simplest terms, is the order in which you complete your full year of core rotations. For example, this could look like OB/GYN to Pediatrics to Surgery to Family Medicine to Psychiatry to Neurology to Internal Medicine. You are with the students in your track from September to September as the year progresses, and these are the people you see the most when you have lectures for your rotations or other mandatory clinical duties as a group. It becomes like another little family of students, and a great community to bond over all your clinical experiences with since you’re going through it together!
Your track group also becomes your Near Peer Mentorship group. Mentors for each group typically completed their clinical year on the same track as you, or one that was very similar, so they can provide the best advice for the specific order in which you complete your rotations. The goal of the Near Peer Program is to help guide students through their clinical year. Our mentors help provide study tips and tools, are sources for what to wear on your first day, where to show up, and how to prepare, and serve as a listening ear when a patient encounter or a day with an attending may not go according to plan.
One of the most helpful aspects of the Near Peer Program is the session on Pre-Rounding and SOAP (Subjective, Objective, Assessment, and Plan)-style presentations during TTC. This session is designed to have our senior students walk through what the heck “pre-rounding” is (checking on what happened to your patients over the past 24 hours and overnight, and gathering information to present on rounds) and how to dig through the charts to find all the information you need to give to the team when you round on your patients. It is also always scheduled the week before you start in the clinical space, in order to provide space for students to ask any logistical questions they have about their first day or just get general advice about clinical year.
Throughout the year, there are a few sessions offered with the Near Peer Mentors as check-ins and opportunities to reconnect with the senior students and regroup as the year progresses. Some questions our mentors always get as clinical year continues are study strategies for each shelf exam, how to manage difficult situations on teams, and how to maintain wellness through long hours at the hospital and studying.
Impact of Near Peer on the Clinical Year
One of the perks of having the Near Peer Program as an integrated part of the clinical year experience is that as an M2 student, you don’t have to put in any effort to sign up or find a senior medical student mentor. We provide all the contact information for the multiple Near Peer Mentors assigned to each track and make the study tips and clerkship-related resources easily available and accessible. This means that as a student trying to figure out what is happening on every rotation, you at least do not need to worry about who you can turn to for help, for reassurance or for concerns. There is always someone ready to support you!
We hope the Near Peer Program provides students with a rich community and useful advice as they tackle the next stage of medical school. We are so excited to continue to make sure all our students feel adequately supported and prepared!
by Aseel Haidar | Dec 1, 2022
Calories in < calories out.
For as long as I can remember, I believed that this was singlehandedly the key to achieving any sort of weight loss or treatment for obesity. Ironically, this concept was challenged many times in my own personal weight-loss journey, and yet, I continued to believe that nutrition and exercise alone should cure any weight-related health concern. I was quickly proven wrong when I got together with a group of ambitious M1s (Svati Pazhyanur, Olivia Hazelrigg and Nadia Aboumourad) and Dr. Amal Othman, Medical Director of the University of Michigan Weight Navigation Program (WNP), to create the obesity medicine elective.
Regardless of your medical specialty, every one of us will work with overweight or obese patients. I can almost guarantee that at some point in your practice, you will have a conversation with a patient about weight management. Beyond learning the biochemical pathways related to weight gain and a few nutrition-focused lectures during my M1 year, there was limited practical discussion of obesity within the curriculum. This elective is an opportunity to introduce medical students to the diverse care teams, causes and treatments involved in caring for patients with obesity so they can best navigate those conversations.

Medical Director of the WNP and leader of our team, Dr. Amal Othman
After countless weekly meetings with my team, coordination with doctors, PAs and nutritionists from relevant clinics and programs, and navigating the Individually Arranged Elective process through the medical school, I was ready to rotate through the pilot elective in July 2022. In 4 weeks, I rotated through multiple Weight Navigation Clinics in the department of Family Medicine, the Metabolism, Endocrinology, and Diabetes (MEND) clinic at Domino’s Farms, the Bariatric Surgery Program, the Michigan Interdisciplinary Clinic for Obesity and Reproduction (MICOR), and even multiple virtual support groups out in our community. A busier day could start with scrubbing in to a sleeve gastrectomy with Dr. Nabeel Obeid. In the afternoon, I would head over to Briarwood Family Medicine to see WNP patients with Dr. Gabison. I’d get to see a few patients on my own and also get some great teaching about metabolic syndrome. On my self-study days, I watched a few webinars from experts in the field through the Obesity Medicine Association’s virtual curriculum.
Since July, other medical students have had the chance to rotate through the elective and provide valuable feedback that has helped us improve the course. Our team asked Quintin Solano, M4, if he learned anything during the elective (October 2022) that surprised him.

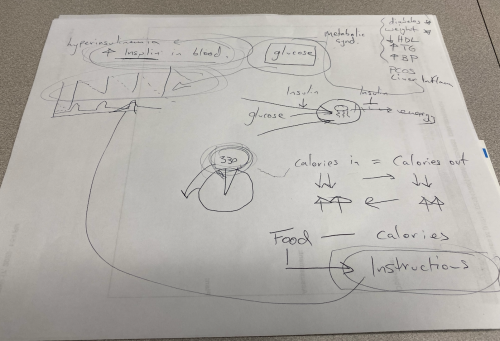
Abed Kawakibi, M4, in Weight Navigation Clinic with Dr. Gabison discussing hyperinsulinism and its effects on weight loss.
“There are many new things I learned during the Obesity Medicine elective. Two that surprised me the most were 1) the medicines we have to treat obesity are very effective and come with a lot of stigma from society as a whole. It is NOT weak or lazy to use medication to treat obesity. The continuous rise in obesity rates across the nation demonstrates how difficult it is to treat obesity. 2) When we ask patients to lose weight, we are asking them to make changes in their personal lives, their families lives and their spouses’ lives. For example, some families show love to each other through food, and we may be asking them to then change how they demonstrate love to one another. Simply saying ‘lose weight’ is minimizing the difficulty that this statement holds.”
To me, the most impactful part of the rotation has been learning to reframe the ways we discuss weight loss with patients. We don’t talk much about calories, exercise routines or restrictive diets. While a calorie deficit is one small piece of the puzzle, there are many other things to consider when counseling a patient about weight.
We first address the underlying medical conditions, both physical and mental, that actively contribute to weight gain. We obtain a comprehensive history of a patient’s experience with obesity and try to understand the factors limiting weight loss. There is always time allotted each visit to provide education about how different foods impact insulin levels, and the nutritional strategies patients can utilize to promote satiety and decrease hyperinsulinism. Finally, we come up with a patient-centered and realistic plan that may incorporate FDA-approved medications for appetite control, behavioral resources and an abundance of high-protein and insulin-friendly foods to choose from. There is no specific numeric goal weight we are trying to achieve, but rather, we strive for improvements in comorbidities and an overall decreasing trend in weight.
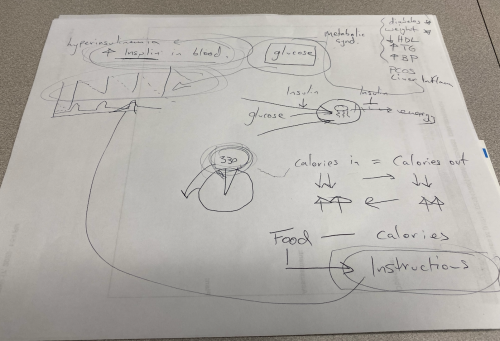
An example of teaching Dr. Gabison does with patients to help reframe weight loss in the context of decreasing insulin levels and improving overall metabolic health.
Perhaps most important of all is the nature or tone of these conversations – there is no judgment or shame. This was nobody’s “fault.” The person seated next to you is trusting you to help improve the quality of their life once and for all. This type of responsibility requires us to check our implicit and explicit biases towards overweight people. We also owe it to our patients to stay up-to-date on current treatments for obesity like we do other medical conditions. It’s these kinds of interactions with patients that energize me as I prepare to begin a career in family medicine.
“Obesity Medicine is a necessary part of medical student education. By 2030, it is projected that over 50% of the United States will have a diagnosis of obesity. Obesity can lead to a plethora of co-morbid disease such as mental health diagnosis, cardiovascular disease, diabetes and many others. We as providers must know how and/or understand when to refer individuals with a diagnosis of obesity for further care. This is not something we can ignore and just say ‘lose weight’ anymore.” – Quintin Solano, M4
Today, approximately 42% of American adults are obese. Weight discrimination in America has increased by nearly 70% in the last decade. The sooner we educate future physicians to overcome our own biases towards weight, as well as identify obesity as a chronic medical condition, the sooner we can help cultivate an attitude of advocacy for our patients with obesity.
If you have any questions about the elective or how you can create your own medical student clinical elective, feel free to email me at jhaidar@umich.edu!
by Sonal Joshi, PhD | Nov 22, 2022
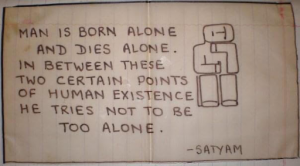 During our childhood trips to India, my sister and I would rummage through the few remaining belongings of our father, anything that would give us a glimpse into who he was. Once, we found a sketch he had made in his teenage years accompanied by the words, “Man is born alone and dies alone. In between these two certain points of human existence he tries not to be too alone.” As we traverse through life, we seek meaning and belonging, to learn from one another, to feel a little less alone.
During our childhood trips to India, my sister and I would rummage through the few remaining belongings of our father, anything that would give us a glimpse into who he was. Once, we found a sketch he had made in his teenage years accompanied by the words, “Man is born alone and dies alone. In between these two certain points of human existence he tries not to be too alone.” As we traverse through life, we seek meaning and belonging, to learn from one another, to feel a little less alone.
Many of us chose medicine for the opportunity to form human connections. However, despite daily interaction, medical school can sometimes be a lonely time. Family and friends who were once a large part of our support network may now have difficulty understanding the challenges we face day to day. Studies have shown that student performance is linked with social bonds, highlighting the importance of connecting with those who can empathize with us. Similar to individual sports, we must rely on our teammates to pump us up along the way; near peers can provide a listening ear, guidance and support. Joining student organizations such as the Association of Women Surgeons can help mitigate that sense of isolation and provide the reassurance we all need.

AWS Board
The Association of Women Surgeons (AWS) at the University of Michigan is a group for individuals who identify as women (and those who support them!) who are interested in learning more about surgery. Our mission is to inform, support and create a united community for women in surgical specialties. We meet monthly for skills nights, panel discussions and casual gatherings, such as ice skating and happy hours. Last August, we hosted a summer series where surgical residents and attendings addressed common questions regarding picking a specialty, balancing work and life, maintaining relationships and having a family. Given the challenges that women often face in surgical specialties, having such panels provide us with mentorship and the sense of community.
 Most recently, we visited the Dexter Cider Mill. Folks brought their loved ones and pups to experience the beautiful Michigan fall colors. Through these AWS events, we hope to create a positive and uplifting community in effort to not feel too alone. We enjoyed donuts while sipping on cider, chatting about everyday life, exams, clerkships and residency interviews. It was lovely to take a quick study break to see old friends and make new ones, and a much needed reminder to get out and connect.
Most recently, we visited the Dexter Cider Mill. Folks brought their loved ones and pups to experience the beautiful Michigan fall colors. Through these AWS events, we hope to create a positive and uplifting community in effort to not feel too alone. We enjoyed donuts while sipping on cider, chatting about everyday life, exams, clerkships and residency interviews. It was lovely to take a quick study break to see old friends and make new ones, and a much needed reminder to get out and connect.
If you are interested in learning more about AWS at the University of Michigan Medical School, please reach out to aws.leadership@med.umich.edu or follow us on Twitter @aws_umich and Instagram @aws.umich for future events. We hope to see you soon!
Read Sonal’s previous blog post: LEADing the Future of Medicine at Michigan
by Devon Cassidy | Oct 27, 2022
I entered medical school with the lofty goal of having an impact on individual patients and populations through medicine, research and policy change. Defining impact is difficult, however following my interests which became passions allowed me to believe I could meet this goal. As a first-year student, I sought opportunities to connect with the community, as most of our time is spent learning about medicine through lectures and not through direct patient care at this point in the curriculum. I began working with the University of Michigan Asylum Collaborative and the Michigan Immigrant Rights Center to provide medical evaluations for those seeking asylum. Medical affidavits documenting the physical and psychosocial signs of human rights abuse and its sequalae can drastically increase the chances of being granting asylum in the U.S. This was impactful work for both me and each person we worked with. However, as I continued to observe injustices play out time and time again for this population, I saw the opportunity to make an impact beyond the individual.
I was introduced to Mateo,* a 25-year-old father and agricultural worker in Michigan, who received a new diagnosis of End Stage Kidney Disease (ESKD). Within days of his initial symptoms, his life was uprooted by his disease, and as his condition worsened hastily, he presented to his local hospital for care. There, he was greeted with a multitude of questions, many of them not pertinent to his symptoms and care, but instead about his citizenship status. After his initial hospitalization and diagnosis, Mateo underwent placement of a temporary central venous catheter, an IV in the large veins of his neck through which he would receive emergency hemodialysis, the only treatment available for his life-threatening diagnosis. Mateo improved rapidly, only to find out that he would need the same treatment three times a week to stay alive. As an undocumented immigrant in the U.S., he could not receive chronic (long-term, ongoing) hemodialysis, the standard of care for ESKD. Instead, Mateo’s discharge plan was to seek dialysis every week when he felt ill enough to come to the emergency department. At 25 and with a family to care for, the prospect of a life of uncertainty was devastating.
Undocumented immigrants residing in the U.S. are dying from ESKD because unjust state legislation is excluding them from accessing life-prolonging interventions such as dialysis and transplantation. Grounded in the firm belief that health care is a human right, I sought to understand the root cause of this problem. At the start of training, medical students are in the position to listen to our patients’ stories and provide a humanistic perspective. We closely observe the societal problems affecting patients in our learning environments, but are rarely placed in a position to help fix them. Training hospitals are not always equipped with the tools to allow students to solve the problems they observe in the clinical environment.
To this point, medical education institutions have a responsibility to decrease the barriers for advocacy engagement for trainees of all levels. I partnered with another medical student, Amalia Gomez-Rexrode, and began to learn more about the systematic nature of this coverage issue. We wondered how we could impact change from our position. We learned that several states had already proposed legislation to ensure these patients have access to life-saving treatment. While this problem was new to us, it was not new to the community or the experts in the field. Our resident and faculty mentors encouraged us to find additional expertise and guidance, and to seek collaborations with community partners. Consistently, we were empowered to take on the task of seeking justice ourselves. Despite common misconceptions about the limited agency of students, no problem is too big, or too bureaucratic, for trainees to become involved in the solution.
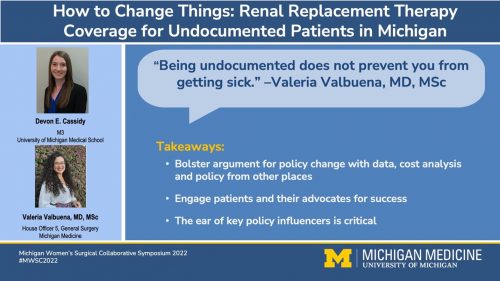 Over two years, we transformed our interest into concrete deliverables including a policy brief, interviews with affected patients, cost analyses, grants and countless meetings with a coalition of attorneys, physicians, community stakeholders and advisors, which helped to shape how we will practice medicine and provide care to all patients. We successfully advocated for a change to Michigan Medicaid, which became effective April 1, 2022. Now, all people in the State of Michigan can access dialysis regardless of immigration status.
Over two years, we transformed our interest into concrete deliverables including a policy brief, interviews with affected patients, cost analyses, grants and countless meetings with a coalition of attorneys, physicians, community stakeholders and advisors, which helped to shape how we will practice medicine and provide care to all patients. We successfully advocated for a change to Michigan Medicaid, which became effective April 1, 2022. Now, all people in the State of Michigan can access dialysis regardless of immigration status.
The Michigan Capstone for Impact (CFI) curriculum was developed for students to explore what they are most fundamentally passionate about. This work uniquely combined my interests of working with the Asylum Collaborative, transplantation health services research and health policy. I had opportunities to work with leaders in diverse fields and gain knowledge that will be critical to being an effective patient and policy advocate going forward in my career. Fighting for change shaped my medical education and gave me a unique perspective to experience the forces of the larger system that surrounds us all. By centering advocacy in my life as a budding clinician, I plan to continue to build space into my future practice to fight for patients and empower others to do the same.
There will never be a better time to learn and grow as an advocate than to start now. When an issue feels larger than yourself as a trainee, it might be one most worth trying to fix.
Acknowledgements: Thank you to Dr. Valeria Valbuena (General Surgery PGY6), Amalia Gomez-Rexrode (M4), Dr. Michael Englesbe (Department of Transplantation Surgery) and all of our community partners who none of this work would be possible without.
*Name and details have been changed.
by Aurelio Muzaurieta | Sep 22, 2022
“Study abroad” isn’t something most students can say they did in medical school. This summer I had the opportunity to rotate in Brazil entirely in Portuguese to bolster my language skills and cultural humility to serve Portuguese-speaking patients. This experience was part of my broader goal to serve patients in their preferred language and to build an impactful career in global health.

At the entrance of the Orthopaedics and Traumatology Institute, affiliate of the Hospital das Clínicas and University of São Paulo School of Medicine.
It has been estimated that more than 25 million people in the United States have limited English proficiency and regularly struggle to communicate with their health care providers. As the United States becomes more linguistically diverse, our health care system must continue to adapt to serve the country.
The desire to serve patients with limited English proficiency is one of my strongest motivators for entering the medical profession. I grew up in a bilingual household where my grandmother, who immigrated from Cuba and never felt confident in English, always felt uncomfortable seeing physicians who did not speak Spanish. The fact that mastery of a patient’s preferred language not only improves clinical efficiency and quality of care but also enriches the patient-physician relationship has inspired me to study world languages and global health care systems.
As an undergraduate at Harvard, more than half of my courses were in foreign languages: Spanish, French, Portuguese or Mandarin Chinese. I took literature and history courses about the lands where these languages are spoken alongside organic chemistry, biology and physics with the hope of one day bringing them together in service to patients. I volunteered as a multilingual interpreter at Massachusetts General Hospital and spent a summer researching the Zika Virus in Brazil during the 2016 Olympic games. I spent time at clinics, shelters and food banks in the Boston-area that served predominantly Portuguese-speaking communities. Not only did these include Brazilians, but also immigrants from rural Portugal, Cape Verde, Angola, Mozambique, and São Tomé and Príncipe. After graduation, I pursued a master’s degree in health economics and management at Peking University in Beijing and wrote a thesis comparing health care systems in America, China and the U.K. My goal in these endeavors abroad was to evaluate the physician and patient experience in diverse health care delivery ecosystems.
When applying to medical school, the opportunity to develop clinical skills in a multilingual context and to pursue global health was a top priority and one of the main reasons I decided to attend University of Michigan Medical School. Not only does our school offer programming in Medical Spanish, Chinese and French, but as a clinical student I applied this skill set in real patient care, especially in the emergency department, primary care clinics, and the Labor and Delivery service during the OB/GYN rotation. Moreover, Michigan’s accelerated pre-clinical phase opens our third and fourth years (called the “Branches”) to customizable clinical, research and entrepreneurial opportunities that are rare at other medical schools. Global REACH, Michigan Medicine’s international office, provides unparalleled administrative and financial support for medical students dedicated to projects pursuing global health equity.
Thanks to the support of Global REACH’s Dr. Joseph Kolars, Dr. Denise Tate and Tania Piotrowski; U-M Orthopedic Surgery Department’s Dr. Jaimo Ahn, Dr. David Walton and Dr. Eileen Crawford; and University of São Paulo’s School of Medicine’s Dr. Júlia D’Andrea Greve and Dr. Linamara Rizzo Battistella, I designed a four-week clinical program in comprehensive musculoskeletal medicine and orthopaedic surgery in São Paulo, Brazil at the Hospital das Clínicas, the largest hospital system in the Western Hemisphere and affiliate of the University of São Paulo School of Medicine (FMUSP).
During my rotation in Brazil, I rotated through operating rooms, inpatient floors and outpatient clinics, including orthopaedic trauma, sports orthopaedics, spinal cord injury, traumatic brain injury and amputations. I also had contact with emergency rooms and primary care clinics to broaden my exposure to the Brazilian health care system as a whole. Rotating in a city as large and dense as São Paulo offers a wide range of clinical scenarios unlikely to be seen in Michigan or even in the United States! For example, one patient presented with cervical spine trauma after a jackfruit – a tropical fruit weighing up to 80lbs – fell from a tree and struck his head while he was strolling on the sidewalk. Culture plays a significant role in medicine as well. Given sport, music and dance are salient features of Brazilian society, clinical research often explores topics in soccer, volleyball, footvolley, Futsal and samba.
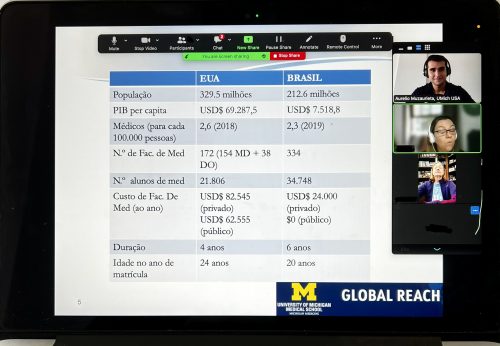
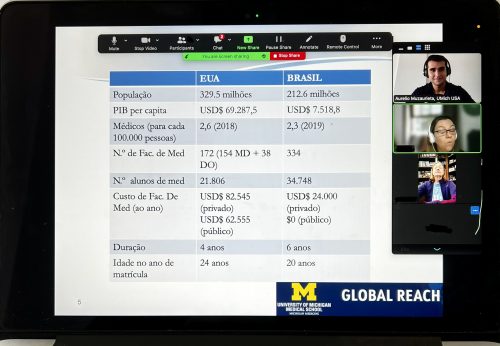
Delivering a virtual presentation in Portuguese on the American Medical Education System to medical students, residents, faculty and researchers at the University of São Paulo Medical School.
My rotation in São Paulo also exposed me to how medicine is studied and practiced in Brazil. Learning about the Brazilian medical education system made me reflect on my educational experience at Michigan and the American system more broadly. At the end of my rotation, I gave a presentation in Portuguese to medical students, residents, attending physicians and researchers about American medical education. We exchanged so many interesting ideas and insights that we decided to build a formal program to connect our institutions at the trainee and faculty level to give continuity to these valuable conversations.
For me, medical school is about becoming the best doctor we can for our future patients. The opportunity to combine the clinical skill set I am learning at Michigan with my Portuguese language skills to care for patients in Brazil was by far the most impactful experience I have had during medical school. Not only did the experience improve my medical Portuguese, but I also feel more nimble navigating new clinical and administrative environments and better equipped to serve patients in high-volume settings. Additionally, given the stark differences in health care infrastructure, building bridges between American and Brazilian medical institutions offers the opportunity to share insights about best clinical practices and systemic design. Rotating at the University of São Paulo motivated me to continue mastering the skills necessary to serve vulnerable patients and to build on my career goals in health care delivery optimization.
I am so grateful for my mentors at the University of Michigan and University of São Paulo who support my academic and professional pursuits. When we say “Go Blue” it truly is a statement of family and community that spans across the globe. I am proud to be a Michigan Wolverine.
I am more than happy to speak with prospective or current students about Michigan. Please do not hesitate to reach out on LinkedIn, Instagram or Twitter!
by University of Michigan Medical Students | Sep 7, 2022
The University of Michigan Medical School’s first “Get to Know Blue” Interview Experience is just around the corner on September 15th.
For those of you with medical school interviews scheduled — and those who hope to have interviews scheduled soon — last year’s incoming class of Michigan med students had put together their best advice for making this day a success for you, too.
Topics range from how to set yourself apart and deciding where to interview to the do’s and don’ts of virtual interviews, getting the inside scoop from current students, and even some bonus tips.
On how best to convey what sets you apart on the spot (or on camera):
- “Oftentimes the things that set you apart don’t have to do with your academic qualifications, but rather your real life and work experiences, and even your hobbies!” -Matthew
- “Have a list of anecdotal examples that highlight who you are and incorporate them into the conversation because they will only learn what you tell them about yourself, so share a lot!” -Gabriela
- “Be yourself, be humble, and be confident. Those three things will give the admissions committee good insight on what makes you unique.” -Miles
- “Just tell your story and be honest. When I messed up on interviews, it was usually because I was trying too hard to tell the interviewer what I thought they wanted to hear.” -Matt
- “Know your story inside out, knowing your unique journey and being able to explain why that story has led you to medicine will automatically set you apart because no one else has your story!” -Navjit
- “Be yourself, stay calm, and don’t worry or feel intimidated by the virtual nature of the interview. The committee is interviewing you not to grill you, but rather because they are super excited to learn more about you!” -Husain
- “You are much more interesting and unique than you may think you are, and if you speak about your true passions, it will come across as genuine.” -Chloe
- “Remember you’re talking to a PERSON not a screen. It can be easy to get stiff on camera but it’s important to relax and be organic.” -Lindsey
- “Invest your time to really understand why you chose medicine and what makes you want to pursue it so much, where your passion for medicine came from and what maintained that interest all this time to continue pursuing it. This will also help you keep your perseverance through medical school.” -Aasma
- “It is hard to convey emotion over a camera but I tried to keep eye contact and just convey that I was truly happy to be part of the interview process. Try your best to just have a normal conversation! You are already halfway there by making it to the interview.” -Hiba
- “Leaning into your passions in an interview and throughout your written application ought to be enough to showcase your awesome-ness to the school that is right for you.” -Lindsay

The White Coat Ceremony for the incoming Class of 2021
On deciding where to interview, especially when travel costs aren’t a consideration:
- “Don’t undersell yourself when applying, if you think you have a chance, take it!” -Niki
- “Interview everywhere possible when travel costs aren’t a consideration. You don’t know how much you may like a school if you don’t choose to even interview and take the chance to explore its culture and environment.” -Aasma
- “I really enjoyed the interview process. It was the first time I felt like people were seeing Sarah the person versus Sarah the numbers on a page. I got to be myself and that is even more available when there are remote interviews.” -Sarah
- “Make sure the school you are interviewing at has resources in what you want to do (very important).” -Bruce
- “Talk to other students or other applicants, if available. Culture is #1. The people who the school recruits say the most about their culture.” -Matt
- “Do your research! You owe it to yourself and the schools interviewing you to make sure that you have spoken with students and faculty about the institution and the experience at their medical school.” -Ashwin
- “Make sure you’re interviewing at schools that FIT you.” -Patrick
“Interview at schools with significant financial aid and/or scholarships. Cost of attendance will be an important consideration when you decide which school to attend.” -Tosin
- “You want to attend an institution that will nurture your passion and develop it into a craft.” -Hebah
- “Notify a school early on if you aren’t considering their school anymore to save interviewers, schools, and other applicants time. Be sure to take advantage of your opportunities while still respecting others in the process.” -Sydney
- “When researching for the interview, I always asked myself if I was excited to learn more about the school or if there was something in particular I was excited about. If not, then I would decide not to interview at the school.” -Hiab
- “You should see every offer as if it is your potential home for the next four years.” -Mohammed
- “If you truly cannot see yourself thriving in the city or your goals for medical school do not align with the mission of the school, do not interview!” -Emily
- “Interview at the places you feel excited about attending! It makes preparing for the interviews enjoyable and your excitement day-of will be genuine.” -Cara
- “Go into the interview open-minded. You never know how much you could see yourself at a specific program if you do not give yourself the opportunity to immerse yourself within the school’s culture.” -Amy
Do’s and don’ts for preparing for and thriving during virtual interviews:
DO’S
Find a Great Place to Set Up
- “Preparing my background and the space where I did virtual interviews really helped me feel prepared.” -Rachel
- “Stay in the same environment for each medical school interview if possible, which will help you remember your anecdotes and release nerves.” -Ashwin
- “Choose a comfortable spot. For me, interviewing from a familiar desk at home improved my performance rather than interviewing from a new location.” -Navjit
- “Investing in a mini ring light if you can afford it can be helpful if you are in a setting with bad or variable lighting, it just looks professional.” -Juliana
- “Use a study/conference room somewhere if you can (work, school, etc.). This helped me move from my home to a more professional setting and got my nerves up a little so I could have an edge while interviewing.” -Sarah
- “Set up your camera to be in good front lighting and put it on a RAISED platform! Having a camera angle pointed straight at your face or even pointed down toward your face makes you look more engaged and is a better angle for aesthetics as well.” -Jayna
- “Give your living-mates ample notice and reminders about your interview days so they can plan ahead about supporting you by keeping the home relatively quiet.” -Lindsay
Dress the Part
- “Wear both a dressy top and bottoms to avoid awkwardness if you need to stand up.” -Josh
- “Wear cozy socks/slippers! A silly tip, but a perk of virtual interviewing that helped me feel much more comfortable during an otherwise stressful situation.” -Anjali
Make Eye Contact
- “Put a picture you like to look at right next to your camera. It made it really easy to look directly at it, even when I was nervous.” -Sarah
- “Looking at the camera isn’t needed if the camera is right above your screen – instead just sit a bit farther away.” -Pratik
- “Virtual eye contact is achieved much more effectively if you look into the computer camera rather than the eyes of the person on screen. It is a little weird to get used to, but you do get used to it!” -Olivia
- “You have to really engage with your interviewer. They don’t have any physical cues and body language is harder to read, so acting interested and really being an active listener is important.” -Mary
Prepare for Potential Tech Issues
- “Prepare for the worst with respect to technology, and be adaptable if something goes wrong.” -Bruce
- “Establish a stable internet connection beforehand and make sure it is steady.” -Sagar
- “Have an ethernet cable nearby in case you need it, and a phone that can be a mobile hotspot if the wifi is bad that day. I ended up using both at some point.” -Lindsey
Practice, Practice, Practice
- “The flow of conversation is simply different. Due to the lag, you may cut someone off or vice versa, this takes some practice and compassion.” -Jasdeep
- “Thoroughly read your application beforehand and learn the format of the interview (1:1 with faculty, MMI, group activity, etc).” -Tosin
- “Google potential questions and do mock interviews with them over and over.” -Noah
- “Use your computer to record yourself answering interview questions and use that to gauge your eye contact, facial expressions, and fluidity of speech (speed, use of “um,” etc.).” -Chloe
- “Always pause and take a breath before answering the question, you don’t want to start talking as soon as the interviewer finishes asking the question.” -Mohammed
- “Take a video of yourself in the setting and outfit you plan to wear for the interview, ask a friend or family member to conduct a practice Zoom with you! This will help you ensure internet connection and Zoom background are updated.” -Emily
Take Breaks
- “Try to take advantage of all breaks possible, Zoom fatigue is very real.” -Hiab
- “HAVE A DANCE PARTY BETWEEN INTERVIEWS! During my interview day I turned on music and my group danced! It was fun and shocked the nerves right out.” -Sarah
- “I would walk around whenever there were breaks because sitting down for that long can be very difficult.” -Hiba
Bring Refreshments
- “Keep yourself hydrated throughout the day to help you reset between interviews.” -Jasdeep
- “I kept small snacks, water, and tea handy, so that I would be able to sneak in a few bites here and there during long Zoom interviews.” -Erin
DON’TS
Don’t Sweat the Tech Issues
- “Don’t panic. The issue will be resolved, and you don’t want to be flustered in your interview.” -Matthew
- “Don’t worry if a technical issue occurs that causes a lag or signs you out of the call. The admissions team are incredibly helpful and they’ll make sure your interview process is as smooth as possible (one of the defining features of my UMMS interview, an incredibly smooth and enjoyable process)!” -Hebah
- “Most importantly: relax and be you. Even if you feel like one part didn’t go well or you are having tech issues, take a deep breath and start fresh. Contact the person you are told to contact when you are having issues and know everything will work out just fine.” -Aasma
- “If you experience a connectivity problem, treat it as a chance to show your interviewer that you can competently handle a difficult or awkward situation.” -Ahab
More Don’ts
- “Don’t hesitate to ask your interviewer to restate a question.” -Jorge
- “Don’t be the person who’s grossly underdressed on interview day or constantly interrupting others (leave room for others to speak).” -Mikaelah
- “Don’t swivel in a spinning office chair. To remove the temptation, I replaced my desk chair with a chair from my kitchen table.” -Jess
- “Don’t spend too much time looking at your own video – it’s distracting! Focus on the videos of the people interviewing you – this simulates a more normal conversation :)” -Cara
- “Don’t forget to smile and breathe! (it is virtual, but I know I still felt very anxious and had to keep reminding myself)
- “Don’t forget to pause at times! With potential delays in the feed, it may take a few moments for one person to stop talking and another to start speaking. This is especially true in group interviews as gaps are needed as a queue for another to start speaking.” -Tyler
- “Don’t look down at notes or at another screen during the interview. While it may be helpful to have notes on hand to remember things you want to mention during the interview, make sure to put them out of sight prior to the interview. The conversation should be natural.” -Amy
On getting the inside scoop from current students at the schools you’re interested in before/during/after you interview:
- “In the virtual format, every perspective matters. Pay special attention to what and how current students talk about their school. If the same complaint keeps showing up, that is probably a red flag.” -Matt
- “I can’t stress enough the importance of sending a few emails ahead of sending your secondaries and during the interview process.” -Ashwin
- “Follow schools’ Twitter and Facebook pages to find opportunities to talk to current students!” -Navjit
- “Almost everyone is very willing to offer advice, they were in the same situation a few short years earlier.” -Mary
- “Seeing whether the students seem relaxed and enthusiastic in answering our questions or hosting the info sessions can also show what type of learning environment and culture the school has. Med school is tough anywhere, but if the students seem happy and relaxed despite the pressure, that’s fantastic.” -Aasma
- “Don’t be afraid to be candid with the students, such as making them know what you are specifically looking for in a school.” -Josh
- “Always ask questions. If in a student-led pre-interview session, have the courage to unmute your microphone and talk to them; that’s what they’re taking time out of their busy schedules to help you with!!” -Mohammed
- “If the school offers an opportunity for you to talk to current students anytime in the interview season, tune in! You don’t have to participate at every one or any, but I found listening in at the very least to be helpful. Seeing how current students interact (their fondness for each other / inside jokes) with each other was reassuring.” -Lindsay
- “Go in with a list of questions around topics/aspects you care deeply about and ask at every school to multiple people if possible. This will give you good points of consensus (or not) within a school and comparison between them.” -Andrea
Bonus tips on the overall application process:
- “It can be very easy to be self-deprecating and compare yourself to others during this process, but surrounding yourself with your supporters can truly make the stress of the application process bearable.” -Amy
- “Enjoy the process, it’s a big step but it’s full of learning experiences and great memories!” -Niki
- “Remember, you are interviewing schools just as much as they are interviewing you!” -Tyler
- “The interview process is the only time an applicant can come alive from a statistic or a piece of paper. Don’t be afraid to vocalize your passion, value, and drive that will distinguish you as a unique asset to the specific medical school and, largely, the field of medicine.” -Erin
- “If you know your interviewer’s name ahead of time, do a bit of research. It was helpful to me to look at a picture of the individual beforehand, so their face was more familiar to me when we were introduced on zoom. It eased my nerves to see a familiar face!” -Cara
- “Be patient!” -Emily
- “When completing an application, answering an essay, or getting interviewed, always be honest and be yourself, that is the one way to get yourself accepted to medical school.” -Mohammed
- “Always stay true to who you are. Trust the process. Remember that everything isn’t always in your control and make the most of the opportunities that present themselves to you.” -Sydney
- “Don’t compromise your happiness. Make sure where you attend you can see yourself being happy, and your interests being valued.” -Aasma
- “See each application and interview as a learning process through which you grow and become even more confident in your capabilities. By the end of it, you’re one step closer to becoming the physician of your dreams. Simply enjoy it.” -Hebah
- “Don’t be afraid to ask for help and advice! Your support system of advisors, family, and/or friends can relieve some of the worries associated with applying to medical school and provide useful feedback.” -Chloe
- “The application process can be daunting, but I think it is really important that you take a step back and look at all that you have done to get to this point. It is truly amazing! No matter how the cycle goes, you can be proud of yourself.” -Olivia
- “Overall, be patient and kind to yourself during the application process. It will feel overwhelming at times, but know that there are people you will encounter along the way who can help you.” -Tosin
- “Don’t ever give up throughout this process. It can be difficult and grueling. I ended up reapplying to medical school after not being accepted my first cycle. I used this additional year to grow, better reflect on my application and have conversations with medical schools across the country. Believe in yourself and keep pushing!” -Ashwin
- “Be genuine! The best thing you can do is present your authentic self. If you’re accepted, you’ll know that the school wanted the authentic you. If you don’t, you shouldn’t have regrets.” -Jasdeep
Good Luck and Go Blue!
 Here at the University of Michigan Medical School, our preclinical education on the basic science necessary to become a doctor is condensed into one year before we dive into the meat of medical school with the clerkship year (check out a full overview of our curriculum)!
Here at the University of Michigan Medical School, our preclinical education on the basic science necessary to become a doctor is condensed into one year before we dive into the meat of medical school with the clerkship year (check out a full overview of our curriculum)!


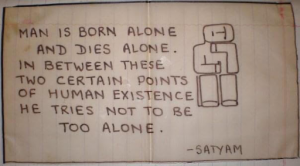 During our childhood trips to India, my sister and I would rummage through the few remaining belongings of our father, anything that would give us a glimpse into who he was. Once, we found a sketch he had made in his teenage years accompanied by the words, “Man is born alone and dies alone. In between these two certain points of human existence he tries not to be too alone.” As we traverse through life, we seek meaning and belonging, to learn from one another, to feel a little less alone.
During our childhood trips to India, my sister and I would rummage through the few remaining belongings of our father, anything that would give us a glimpse into who he was. Once, we found a sketch he had made in his teenage years accompanied by the words, “Man is born alone and dies alone. In between these two certain points of human existence he tries not to be too alone.” As we traverse through life, we seek meaning and belonging, to learn from one another, to feel a little less alone.
 Most recently, we visited the Dexter Cider Mill. Folks brought their loved ones and pups to experience the beautiful Michigan fall colors. Through these AWS events, we hope to create a positive and uplifting community in effort to not feel too alone. We enjoyed donuts while sipping on cider, chatting about everyday life, exams, clerkships and residency interviews. It was lovely to take a quick study break to see old friends and make new ones, and a much needed reminder to get out and connect.
Most recently, we visited the Dexter Cider Mill. Folks brought their loved ones and pups to experience the beautiful Michigan fall colors. Through these AWS events, we hope to create a positive and uplifting community in effort to not feel too alone. We enjoyed donuts while sipping on cider, chatting about everyday life, exams, clerkships and residency interviews. It was lovely to take a quick study break to see old friends and make new ones, and a much needed reminder to get out and connect.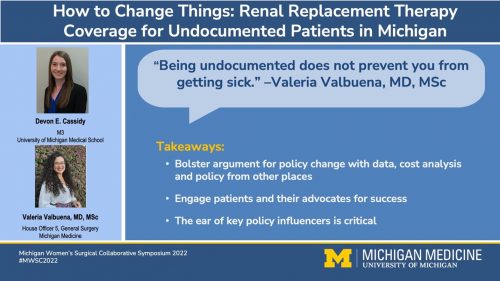 Over two years, we transformed our interest into concrete deliverables including a policy brief, interviews with affected patients, cost analyses, grants and countless meetings with a coalition of attorneys, physicians, community stakeholders and advisors, which helped to shape how we will practice medicine and provide care to all patients. We successfully advocated for a change to Michigan Medicaid, which became effective
Over two years, we transformed our interest into concrete deliverables including a policy brief, interviews with affected patients, cost analyses, grants and countless meetings with a coalition of attorneys, physicians, community stakeholders and advisors, which helped to shape how we will practice medicine and provide care to all patients. We successfully advocated for a change to Michigan Medicaid, which became effective