Calories in < calories out.
For as long as I can remember, I believed that this was singlehandedly the key to achieving any sort of weight loss or treatment for obesity. Ironically, this concept was challenged many times in my own personal weight-loss journey, and yet, I continued to believe that nutrition and exercise alone should cure any weight-related health concern. I was quickly proven wrong when I got together with a group of ambitious M1s (Svati Pazhyanur, Olivia Hazelrigg and Nadia Aboumourad) and Dr. Amal Othman, Medical Director of the University of Michigan Weight Navigation Program (WNP), to create the obesity medicine elective.
Regardless of your medical specialty, every one of us will work with overweight or obese patients. I can almost guarantee that at some point in your practice, you will have a conversation with a patient about weight management. Beyond learning the biochemical pathways related to weight gain and a few nutrition-focused lectures during my M1 year, there was limited practical discussion of obesity within the curriculum. This elective is an opportunity to introduce medical students to the diverse care teams, causes and treatments involved in caring for patients with obesity so they can best navigate those conversations.

Medical Director of the WNP and leader of our team, Dr. Amal Othman
After countless weekly meetings with my team, coordination with doctors, PAs and nutritionists from relevant clinics and programs, and navigating the Individually Arranged Elective process through the medical school, I was ready to rotate through the pilot elective in July 2022. In 4 weeks, I rotated through multiple Weight Navigation Clinics in the department of Family Medicine, the Metabolism, Endocrinology, and Diabetes (MEND) clinic at Domino’s Farms, the Bariatric Surgery Program, the Michigan Interdisciplinary Clinic for Obesity and Reproduction (MICOR), and even multiple virtual support groups out in our community. A busier day could start with scrubbing in to a sleeve gastrectomy with Dr. Nabeel Obeid. In the afternoon, I would head over to Briarwood Family Medicine to see WNP patients with Dr. Gabison. I’d get to see a few patients on my own and also get some great teaching about metabolic syndrome. On my self-study days, I watched a few webinars from experts in the field through the Obesity Medicine Association’s virtual curriculum.
Since July, other medical students have had the chance to rotate through the elective and provide valuable feedback that has helped us improve the course. Our team asked Quintin Solano, M4, if he learned anything during the elective (October 2022) that surprised him.

Abed Kawakibi, M4, in Weight Navigation Clinic with Dr. Gabison discussing hyperinsulinism and its effects on weight loss.
“There are many new things I learned during the Obesity Medicine elective. Two that surprised me the most were 1) the medicines we have to treat obesity are very effective and come with a lot of stigma from society as a whole. It is NOT weak or lazy to use medication to treat obesity. The continuous rise in obesity rates across the nation demonstrates how difficult it is to treat obesity. 2) When we ask patients to lose weight, we are asking them to make changes in their personal lives, their families lives and their spouses’ lives. For example, some families show love to each other through food, and we may be asking them to then change how they demonstrate love to one another. Simply saying ‘lose weight’ is minimizing the difficulty that this statement holds.”
To me, the most impactful part of the rotation has been learning to reframe the ways we discuss weight loss with patients. We don’t talk much about calories, exercise routines or restrictive diets. While a calorie deficit is one small piece of the puzzle, there are many other things to consider when counseling a patient about weight.
We first address the underlying medical conditions, both physical and mental, that actively contribute to weight gain. We obtain a comprehensive history of a patient’s experience with obesity and try to understand the factors limiting weight loss. There is always time allotted each visit to provide education about how different foods impact insulin levels, and the nutritional strategies patients can utilize to promote satiety and decrease hyperinsulinism. Finally, we come up with a patient-centered and realistic plan that may incorporate FDA-approved medications for appetite control, behavioral resources and an abundance of high-protein and insulin-friendly foods to choose from. There is no specific numeric goal weight we are trying to achieve, but rather, we strive for improvements in comorbidities and an overall decreasing trend in weight.
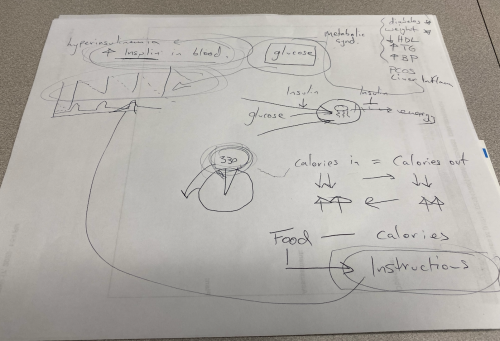
An example of teaching Dr. Gabison does with patients to help reframe weight loss in the context of decreasing insulin levels and improving overall metabolic health.
Perhaps most important of all is the nature or tone of these conversations – there is no judgment or shame. This was nobody’s “fault.” The person seated next to you is trusting you to help improve the quality of their life once and for all. This type of responsibility requires us to check our implicit and explicit biases towards overweight people. We also owe it to our patients to stay up-to-date on current treatments for obesity like we do other medical conditions. It’s these kinds of interactions with patients that energize me as I prepare to begin a career in family medicine.
“Obesity Medicine is a necessary part of medical student education. By 2030, it is projected that over 50% of the United States will have a diagnosis of obesity. Obesity can lead to a plethora of co-morbid disease such as mental health diagnosis, cardiovascular disease, diabetes and many others. We as providers must know how and/or understand when to refer individuals with a diagnosis of obesity for further care. This is not something we can ignore and just say ‘lose weight’ anymore.” – Quintin Solano, M4
Today, approximately 42% of American adults are obese. Weight discrimination in America has increased by nearly 70% in the last decade. The sooner we educate future physicians to overcome our own biases towards weight, as well as identify obesity as a chronic medical condition, the sooner we can help cultivate an attitude of advocacy for our patients with obesity.
If you have any questions about the elective or how you can create your own medical student clinical elective, feel free to email me at jhaidar@umich.edu!
Don’t miss the next Dose of Reality.
Aseel is a fourth-year medical student at University of Michigan Medical School and is currently applying into family medicine. Her professional interests include full-scope family med, primary care gynecology and obesity medicine. When not at school, she can be found practicing dabke, walking a dog or hosting a gathering with her friends!
